What you need to know about the 2021 curriculum

From August 2021, surgical training became outcomes-based. Trainees are now assessed against the fundamental capabilities required of consultants. The end of training is reached when supervisors agree that a trainee is performing at the level of a day-one consultant, successfully managing the unselected emergency take, clinics and ward-care, operating lists and multi-disciplinary working while demonstrating the generic professional behaviours required of all doctors.
At the heart of these changes is the principle that the knowledge and skills essential for everyday practice are reflected authentically in the assessment system. The previous curriculum had attracted criticism for relying too heavily on competency-based training with not enough emphasis placed on the holistic professional judgement of clinical supervisors. Because of this, there is a new assessment called the Multiple Consultant Report (MCR) encompassing the new concepts of the Generic Professional Capabilities (GPCs) and Capabilities in Practice (CiPs).
This curriculum change is the result of new standards for curricula introduced by the General Medical Council (GMC); Excellence by design and the Shape of Training Review. It follows a lengthy consultation process with input from trainees and trainers and contributions from a wide range of stakeholders including NHS employers, service and education providers, patient and lay groups, statutory education bodies and experts in curriculum and assessment design. We are very grateful to everyone who worked with us to make these improvements.
The new curricula are approved by the GMC as the UK framework for surgical training and are also in use for specialty training in the Republic of Ireland. Training is truly capability-based and, although there are indicative times in which the great majority of trainees are expected to complete training, trainees will be able to progress faster through training if they demonstrate the necessary capability.
Whatever your role, trainee or trainer, the curriculum changes affect you.
You can familiarise yourself with the MCR by downloading the step guide and watching the short videos below which explain the process of the MCR. Trainees may also find the general guidance on self-assessment useful before trying out the self-assessment.
Online drop in sessions - Ask Keith
|

Keith Jones, ISCP Surgical Director
|
Ask Keith
Keith Jones, ISCP Surgical Director holds, from time to time, online drop-in sessions on the new curriculum for trainees and trainers. These sessions provide an opportunity for you to ask questions about the new curriculum. They are available from 9am to 10am on certain Fridays. We look forward to meeting you.
More dates to be confirmed. Please refer to the JCST YouTube channel here for further guidance
|
Ask Keith Q&A
Q&A video July 2023
Full video (52.47)
See the summary of points or watch each Q&A below:
What are the most important areas of the curriculum that trainees need to be aware of? (3.11)
What is the best way of carrying out an MCR assessment? (9.59)
What is the meaning of CiP 5, Multidisciplinary Working, and how can it be evidenced? (3.10)
What is the benefit for trainees in doing a Self-Assessment? (5.39)
What is expected of trainees in the Self-Assessment? (2.27)
What impact should the trainee's Self-Assessment have on the MCR process? (3.57)
How do we use WBAs now? (8.53)
Is the midpoint MCR really necessary? (6.31)
Why do trainees need to do an MSF as well as an MCR? (6.29)
Q&A from ISCP drop in sessions
How soon do Clinical Supervisors need to start the MCR after the start of the academic year?
The first MCR takes place at the midpoint of the placement. It needs to be completed at least 2-3 weeks in advance of the midpoint learning agreement meeting.
At the beginning of the learning agreement, the trainee and Assigned Educational Supervisor select a Lead Clinical Supervisor for the MCR before they begin the objective setting meeting. The Lead Clinical Supervisor is able to start the MCR as soon as the objective-setting meeting has been signed off. The MCR should be completed at least 2 weeks before the midpoint learning agreement meeting. Approximate timings for the MCR and Learning Agreement are shown below.
| Approximate timings |
| |
Midpoint MCR |
Midpoint LA |
Final MCR |
Final LA |
| 4-month placements |
End of month 2
(2-3 weeks before midpoint LA) |
Beginning of month 3 |
End of month 3
(2-3 weeks before final LA) |
Middle of month 4 |
| 6-month placements |
End of month 3
(2-3 weeks before midpoint LA) |
Beginning of month 4 |
End of month 5
(2-3 weeks before final LA) |
Middle of month 6 |
| 12-month placements |
Optimal if divided into two 6-month placements and timed as above |
End of month 6
(2-3 weeks before midpoint LA) |
Beginning of month 7 |
End of month 11
(2-3 weeks before final LA) |
Middle of month 12 |
Would trainee presence at the MCR meeting increase transparency?
The MCR meeting enables Clinical Supervisors to discuss their experiences of trainees and share their professional opinions about trainee performance to form a collective judgement. These discussions formalise the informal faculty meetings that have always occurred. The process of arriving at a collective judgement would not be improved by the presence of trainees and transparency is better achieved through trainees being able to assess themselves against the same framework of CiPs and GPCs and in receiving the dedicated feedback afterwards.
Does an Assigned Educational Supervisor’s time commitment need to be longer than a Clinical Supervisor’s?
Assigned Educational Supervisors take responsibility for a trainee’s educational development and for providing reports on trainee progression. They, therefore, need to develop an understanding of how the trainee is progressing over time in different activities and settings and their time commitment is likely to be more intensive over the course of the placement.
Who is responsible for rolling out the curriculum in District General Hospitals?
Everyone who is involved in training should take part in implementing the new curriculum locally via events such as local training meetings, trainee specialty inductions and unit inductions. Trainers who have undertaken ISCP webinar training (including SAC Liaison Members, College Tutors, Training Programme Directors and Directors of Medical Education) will have received a pack of resources to assist in this process.
August 2021 curricula
Cardiothoracic Surgery
Congenital Cardiac Surgery
Core Surgical Training
General Surgery
Neurosurgery
Oral & Maxillofacial Surgery
Otolaryngology
Paediatric Surgery
Plastic Surgery
Trauma & Orthopaedic Surgery
Urology
Vascular Surgery
Key changes
The following are the key changes:
- Training is arranged in phases
- Trainees are assessed through the MCR
- Generic Professional Capabilities carry equal weight to the CiPs
- Capabilities in Practice indicate the end-point of training
- Supervision levels indicate when a trainee is ready to complete training
- The learning agreement focuses training on outcomes
- The role of Workplace Based Assessments is re-balanced
- New transition arrangements apply
Training is arranged in phases
Surgical training is arranged into three phases, each phase having a critical progression point at its end, where evidence of acquisition of capability to a level described in the curriculum is necessary for progression to the next phase or for certification. Details differ slightly between specialties and you should view the specialty curriculum you wish to follow for specific details.
Phase 1: The outcome is to gain the competencies equivalent to those described in the core surgical training curriculum, or the parts of the core surgical training curriculum necessary to progress into the StR role. For most specialties the indicative time for phase 1 is two years.
Phase 2: The outcome is to gain experience in the breadth of the specialty, including the unselected emergency take. If the specialty curriculum describes special interests there are opportunities for early exposure to these to help trainees decide what special interest to pursue later in training. The knowledge, clinical and professional skills are developed to that required of a day-one consultant by the end of phase 2, which make those reaching the end of phase 2 eligible to apply to take the Intercollegiate Specialty Board examination in their specialty. Technical skills are developed throughout the breadth of the specialty, including in emergency cases, but it is recognised that technical skills may develop more slowly than knowledge, clinical and professional skills and so do not need to be at the level of a day-one consultant by the end of phase 2. For most specialties the indicative time for phase 2 is four years.
Phase 3: The outcome is to have gained all the capabilities necessary for safe practice as a day-one consultant in the specialty. As knowledge, clinical and professional skills have been developed to the level of a day-one consultant as part of the outcome of phase 2, then phase 3 allows development of technical skills to the level of a day-on consultant in the generality of the specialty, emergency care and in any special interest described by the specialty curriculum. Once these capabilities have been achieved an Annual Review of Competence Progression (ARCP) outcome 6 may be awarded and trainees can apply for certification.
Please consult the specialty specific training pathways for specific details here.
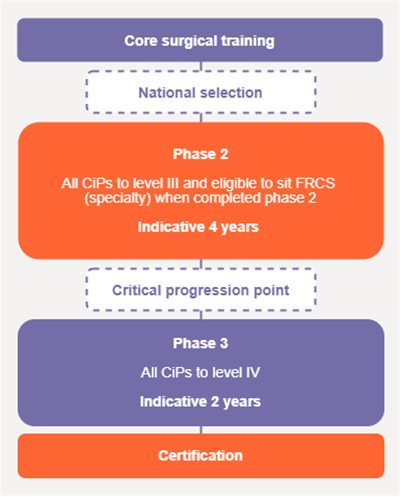
Figure 1: typical phases of a surgical training pathway.
Trainees are assessed through the MCR
The assessment system is made up of several different types of assessment needed to meet the requirements of the curriculum; workplace-based assessments, examinations at key stages and the ARCP. Together these generate the evidence required for global judgements to be made about satisfactory trainee performance, progression in, and at completion of, training. Assessment takes place throughout the training programme to allow trainees to continually gather evidence of learning and to provide formative feedback to the trainee to aid progression.
The MCR is the primary assessment in the workplace, which, together with the other mandatory assessments, is used by the trainee’s Assigned Educational Supervisor to make an end of placement report which feeds into the information presented to the ARCP.
The MCR takes place just before the mid-point and end-point of each placement, ahead of the midpoint and final learning agreement meetings. The clinical supervisors who work with trainees on a day-to-day basis assess them against the high-level outcomes of the curriculum; the GPCs and the CiPs.
Clinical supervisors meet just before the mid-point and end of a placement to discuss the supervision level reached by a trainee in each of the CiPs and also whether trainees are developing GPCs to an appropriate level for the phase of training. If a trainee has not reached supervision level IV or V in a CiP then the MCR requires trainers to identify areas most in need of development in the next three to six months of training in order for the trainee to progress towards a day-one consultant. Trainees complete a form identical to the MCR as a self-assessment and identify their own supervision level and areas for development. If performance is beyond that expected then this can be captured too.
After the assessment, the Lead Clinical Supervisor or Assigned Educational Supervisor should meet with the trainee to discuss the MCR and the self-assessment and agree how to best to develop in the areas identified. This may involve changing the emphasis of the placement slightly if one CiP seems to be falling behind the rate of development in others.
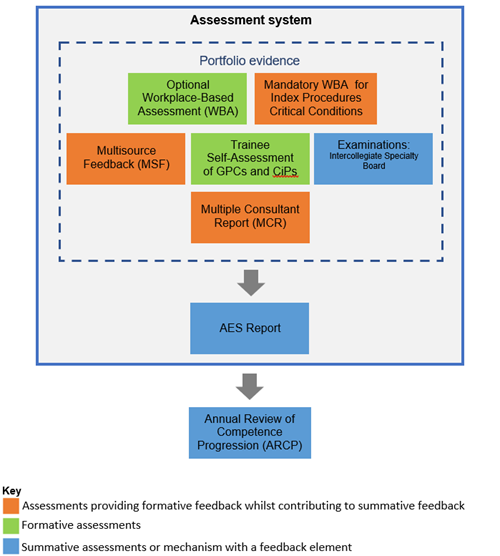
Figure 2: The assessment system
|
|
Introduction to the multiple consultant report
This video expands on how the main change to the assessment system is the addition of a new assessment based in the workplace called the Multiple Consultant Report (MCR). The MCR takes place at the mid-point and end-point of each placement and feeds into the Learning Agreement.
MCR video transcript
|
Generic Professional Capabilities carry equal weight to CiPs
The GPCs describe the interdependent essential capabilities that underpin professional medical practice. They also serve as educational outcomes, carrying equal weight to the CiPs and are, therefore, an integral part of the surgical curriculum, supporting every phase of training.
Satisfactory achievement of the GPCs is assessed through the MCR. Trainees need to demonstrate that they have attained the necessary generic professional capabilities required to provide safe, effective and high quality medical care.
The GPC framework was developed by the General Medical Council and the Academy of Medical Royal Colleges with the aim of providing a consistent approach to ensuring that all doctors demonstrate an appropriate and mature professional identity. The framework prioritises themes, such as patient safety, quality improvement, safeguarding vulnerable groups, health promotion, leadership, team working, and other fundamental aspects of professional behaviour and practice.
|
|
Introduction to the generic professional capabilities
This video talks about how the GPC framework was developed by the GMC and the Academy of Medical Royal Colleges with the aim of providing a consistent approach to ensuring that all doctors demonstrate an appropriate and mature professional identity.
GPCs video transcript
|
Capabilities in Practice indicate the end-point of training
The CiPs are high-level outcomes of training and are aimed at helping trainees to better understand what is expected of them in their training programme. Each CiP covers everything a day-one consultant needs to be able to perform in the main area of the job, integrating the knowledge, clinical, professional and technical skills into a functioning whole.
The CiPs operationalise and contextualise the syllabus under the main activities needed for independent practice at the level of a day-one consultant. They are, therefore, broader than the syllabus and replace the syllabus as the main focus of the MCR. When trainees are assessed as able to perform these essential activities independently then they are considered safe and ready for certification and eligible for a consultant post.
Capability at the level of a day-one consultant has to be reached in all areas of the job to finish training.
There are five CiPs common to all surgical specialties, these are:
| 1) |
Manages an out-patient clinic |
| 2) |
Manages the unselected emergency take |
| 3) |
Manages ward rounds and the on-going care of in-patients |
| 4) |
Manages an operating list |
| 5) |
Manages multi-disciplinary working |
Cardiothoracic Surgery, Paediatric Surgery and Plastic Surgery have additional CiPs because of the different scope of work, these are:
| Cardiothoracic Surgery |
6)
7) |
Manages patients within the critical care area
Assesses surgical outcomes both at a personal and unit level |
| Paediatric Surgery |
6) |
Assesses and manages an infant or child in a NICU/PICU environment |
|
Plastic
Surgery
|
6) |
Safely assimilates new technologies and advancing techniques in the field of Plastic Surgery into practice |
|
|
Introduction to capabilities in practice
This video explains how the new curriculum describes fewer, high-level outcomes of training called Capabilities in Practice (CiPs) aimed at helping trainees to better understand what is expected of them in their training programme.
CiPs video transcript
|
Find out more about the five common CiPs here.
Supervision levels indicate when a trainee is ready to complete training
Through the MCR, the clinical supervisors who work with the trainee on a day to day basis recommend supervision levels classifying how much supervision is required by the trainee in each CiP for the particular phase of training.
To allocate a supervision level ask; ‘how much supervision is needed in this area of work?’ When someone is at the start of training they will need to be supervised more than someone near the end of training. The level of a day-one consultant is reached when no supervision is needed and training can end. The table below sets out each supervision level and its definition for both specialty training and core surgical training. Supervision level I describes someone who can only observe the task and supervision level IV indicates that someone is displaying capabilities at the level of a day-one consultant.
Table 1: Supervision levels describing the level of capability in practice for specialty training
| Supervision Level I: |
Able to observe only: no execution. |
| Supervision Level IIa: |
Able and trusted to act with direct supervision: The supervisor needs to be physically present throughout the activity to provide direct supervision. |
| Supervision Level IIb: |
Able and trusted to act with direct supervision: The supervisor needs to be physically present for part of the activity.
The supervisor needs to guide all aspects of the activity. This guidance may partly be given from another setting.
|
| Supervision Level III: |
Able and trusted to act with indirect supervision: The supervisor may be required to be physically present on occasion.
The supervisor does not need to guide all aspects of the activity. For those aspects which do need guidance, this may be given from another setting.
|
| Supervision Level IV: |
Able and trusted to act at the level of a day-one consultant. |
| Supervision Level V: |
Able and trusted to act at a level beyond that expected of a day-one consultant. |
Table 2: Supervision levels describing the level of capability in practice for core surgical training.
| Supervision Level Ia: |
Able to observe passively only. |
| Supervision Level Ib: |
Able to observe actively: may engage in the activity to provide assistance or analyse and discuss what is observed. |
| Supervision Level IIa: |
Able and trusted to act with direct supervision: some of the activity is performed by the trainee. |
| Supervision Level IIb: |
Able and trusted to act with direct supervision: the trainee is able to string elements together into fluent parts of the task. |
| Supervision Level IIc: |
Able and trusted to act with direct supervision: the trainee is able to complete the task. |
| Supervision Level III: |
Able and trusted to act with indirect supervision: the supervisor will want to provide guidance for, and oversight of, most aspects of the activity. Guidance may be remote or provided in advance of the activity. |
The learning agreement focuses training on outcomes
The learning agreement is structured to allow objectives to be focused on progression through the CiPs and GPCs. The latest MCR as well as the trainee’s self-assessment is displayed to facilitate the setting of goals for the new placement. In this way it is easier to ‘hit the ground running’ in a new placement. Progress towards the objectives set, is reviewed at the mid-point learning agreement meeting along with the formative mid-point MCR and modifications made accordingly. The final review meeting of the learning agreement considers the end of placement MCR. The AES report takes into consideration progress against objectives as well as the MCR and other portfolio evidence for consideration by the ARCP panel at the end of the training year.
The role of Workplace Based Assessments is re-balanced
Because the MCR helps to develop integrated capability in the daily tasks of the job of a consultant surgeon, and to avoid adding another layer of assessment to training, there is no requirement to complete a certain number of WBAs per training year. WBAs remain however, providing additional evidence of competence by the completion of training in key areas of the syllabus; the critical conditions and index procedures. They can also be used by trainees to formalise and structure feedback on particular clinical interactions or procedures if they wish. In addition, they can be used to assess progress towards achievement of targeted training.
The new curriculum allows experience of critical conditions and index procedures to be linked with CBDs/CEXs and PBAs respectively to aid the recording of the breadth and depth of learning.
New transition arrangements apply
From August 2021, trainees should have transitioned to the new curriculum as they moved into the next level of training, exceptions are shown in Table 3 below. All trainees must transfer to the new curriculum by 2 August 2023.
Table 3: Arrangements for transitioning to the new curriculum
|
Level of training to be entered on or after 4 August 2021
|
Required to transfer
|
Deadline for transfer
|
| CT1/ST1 |
Yes |
Not applicable |
| CT2/ST2 |
No but they can if they wish |
If not completed CT2/ST2 by 2 August 2023 will need to transfer |
| ST2 (Neurosurgery) |
Yes |
2 August 2023 |
| ST3 |
Yes |
2 August 2023 (for run through trainees only)
Uncoupled trainees entering ST3 start their specialty training on the new curriculum
|
|
ST4-ST61
ST4-ST72 |
Yes |
2 August 2023 |
|
ST71
ST82 |
No but they can if they wish |
2 August 2023 (if still in training) |
| Less than full time |
Yes |
Trainees who in are less than full time training may remain on the previous curriculum until they transition to the next training level.
All trainees must transfer by 2 August 2023
|
| Out of training |
Yes |
Trainees who take time out of Out of Programme may remain on the previous curriculum while on their current training level. For example, a trainee returning from OOP at ST4 in August 2021 may remain on the previous curriculum until they move to ST5.
All trainees must transfer by 2 August 2023
|
| Training Interface Groups |
No but they can if they wish |
After July/August 2022 Training Interface Group (TIG) Fellowships will become Post-Certification Fellowships.
- The last pre-certification TIG fellows will be recruited in 2020/21 for an August 2021 start.
- The last pre-certification fellows will finish in July/August 2022.
- TIG fellows recruited in 2021/22 for an August 2022 start will be post-certification when they start the fellowship.
|
| CESR |
Yes |
CESR applicants should demonstrate equivalence to the 2021 curriculum. See the GMC’s website. More details about CESR and the new curriculum can be found here.
|
1 Specialties that complete training at end of ST7
2 Specialties that complete training at end of ST8
Notes:
Impact of transferring to the new curriculum:
- Trainees who are required to transfer should do so as they start a new training year on or after 4 August 2021, regardless of the outcome of their preceding ARCP.
Trainees who are not required to transfer may choose to do so if they wish after discussion with their TPD. The notes below describe the impact of transfer if they do.
- Trainees need to learn and demonstrate the Capabilities in Practice and Generic Professional Capabilities through the Multiple Consultant Report.
- There are no requirements to complete a certain number of Workplace Based Assessments (WBAs) per year. WBAs are used to assess critical conditions and index procedures as described in the curriculum, or to assess areas of concern.
- Trainees need to be familiar with and follow a phased training pathway as described in the new curriculum.
CESR applicants need to demonstrate the Capabilities in Practice and Generic Professional Capabilities through the Multiple Consultant Report or equivalent portfolio evidence – see CESR section of the JCST website.
Summary
All medical curricula, including those for surgical specialties, are now outcomes based: a trainee finishes training when they are ready to be a day-one consultant. Clinical supervisors decide when a trainee has displayed the competence required for day-one consultant practice in each area of the working week (the CiPs) and the generic professional capabilities required of all doctors (the GPCs). When this level has been reached, as well as completion of other certification requirements, an ARCP outcome 6 can be awarded and the trainee can apply to be on the specialist register.
Formative feedback improves through the MCR and trainees are more easily able to gain insight into their own performance and training requirements through self-assessment. You can try out the MCR or trainee Self-Assessment - see our FAQ.
>